Subfertility is defined as the inability to achieve a clinical pregnancy after 12 months of unprotected “regular intercourse.” When talking about “regular intercourse,” the frequency of intercourse and its temporal relationship to ovulation must be taken into account.
Regarding frequency, it has been shown that the cumulative probability of pregnancy at one year increases when there are at least two coital relations per week (Table 1). (1) (2)
| Woman’s age | intercourse 2/week | Intercourse 1/week |
| 19 to 26 years | 8% | 15% |
| 27 to 34 years | 13-14% | 22-24% |
| 35 to 39 years | 18% | 29% |
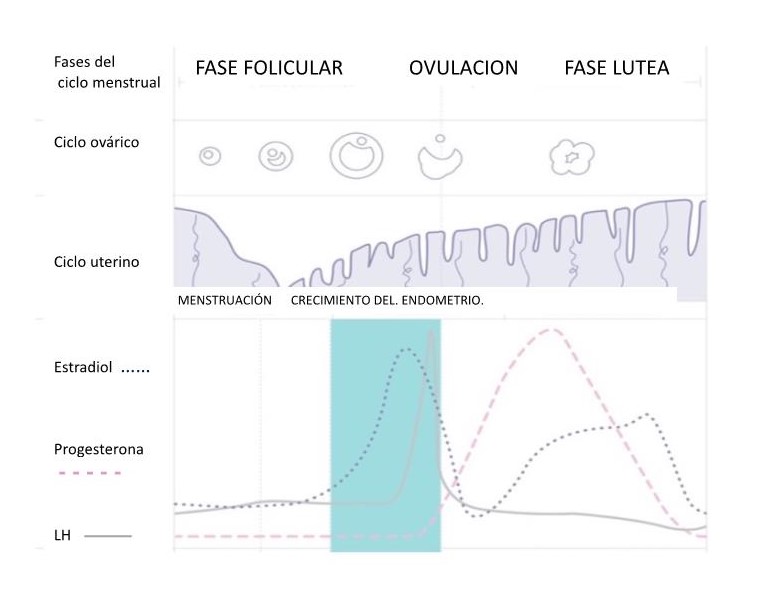
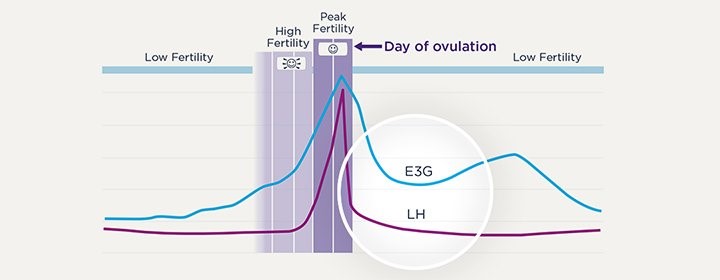
Regarding timing, it has been documented that incorrect scheduling of coital relations with respect to the woman’s fertile days during the menstrual cycle affects the probability of pregnancy. The fertile days in which unprotected intercourse can result in conception are known as the “fertility window.” Although there is consensus that the fertility window ends on the day of ovulation, its start and therefore its duration varies between couples, with a range between
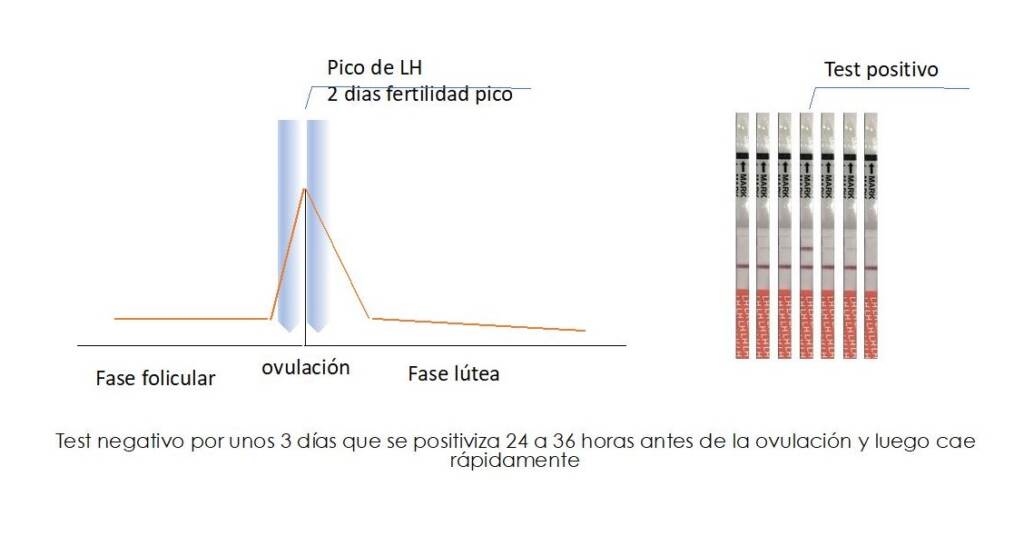
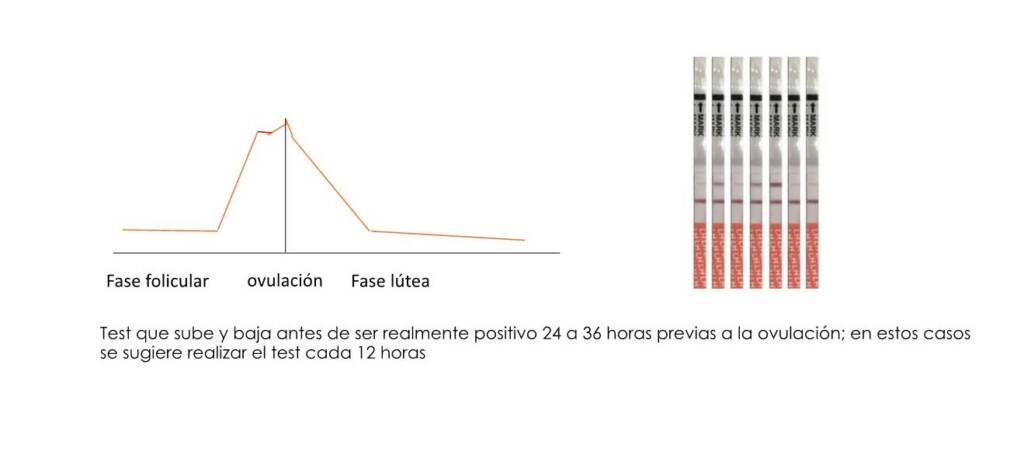
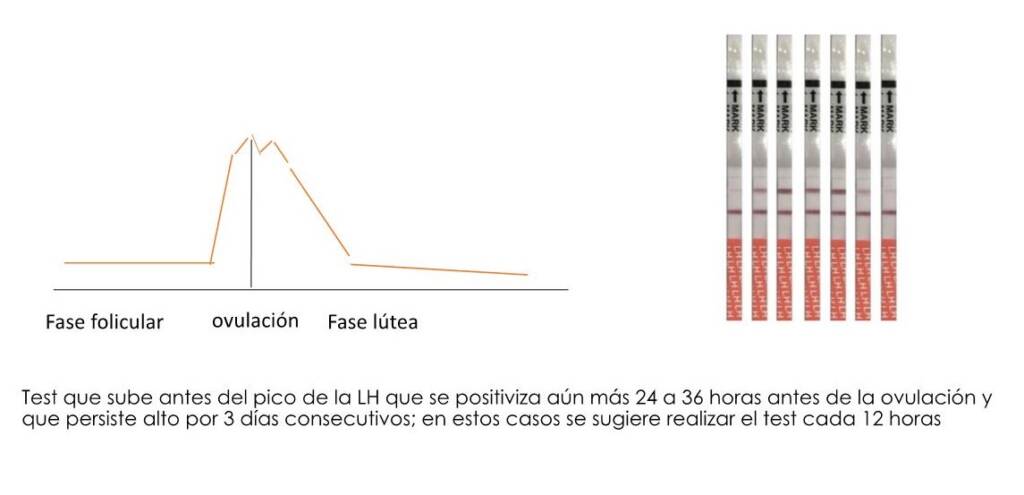
“Timed intercourse” is based on the ability to prospectively detect this fertility window and thus maximize the probability of conception. (4) Most women ovulate about 14 days before the first day of menstrual bleeding. However, because there is a high variation in the duration of menstrual cycles (counting from the first day of bleeding to the day before the next menstruation) between women and even in the same woman, the sole use of the menstrual calendar can be a fairly inaccurate method of predicting ovulation.
Transvaginal ultrasound performed by trained clinical personnel is the gold standard for establishing the time of ovulation. However, there are practical and economical home methods that can predict the fertile period in a large percentage of women.
These include measuring hormones in the urine such as luteinizing hormone (LH) and estrogens; tracking basal body temperature; and evaluating cervical mucus and saliva.
It is therefore important to review the pros and cons of each of these methods and the devices available on the market for their measurement so that women who start trying to get pregnant have a greater probability of achieving conception efficiently.
The popularity of web-based applications for detecting fertile days with software for use on smartphones is increasing. Although most of these applications are only based on the duration of menstrual cycles and the date of the last menstruation, there are already some that incorporate hormonal analysis, and/or monitoring of body temperature. (5)
Conclusion
There are different complementary alternatives that help predict the window and the maximum peak of fertility in addition to the length and duration of menstrual cycles with web-based applications. The information saved through these applications can assist in the medical management of patients who desire pregnancy. Failure to detect ovulation for three consecutive months or failure to conceive after 6 months of timed intercourse through applications that objectively detect the fertility window may be an indication to expedite the study process of a woman and her partner