Fertilización In Vitro ( FIV)
La Fertilización In Vitro (FIV) es una de las técnicas de reproducción asistida más efectivas y utilizadas en todo el mundo. Desde que en 1978 nació el primer bebé mediante este tratamiento, conocido como Louise Brown, miles de parejas han recurrido a la FIV como una alternativa para lograr un embarazo. Esta revolucionaria técnica ha cambiado por completo el panorama de la ciencia y la medicina reproductiva, permitiendo que muchas personas que antes no podían concebir de manera natural, ahora tengan la oportunidad de ser padres.
¿Qué es la Fertilización In Vitro?
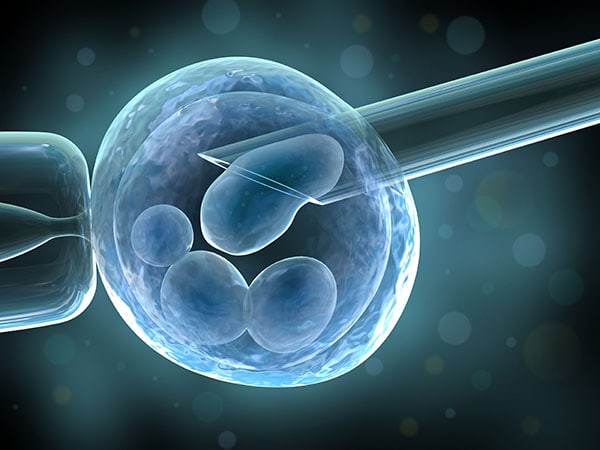
La Fertilización In Vitro es un procedimiento médico que implica la fertilización del óvulo de una mujer con el esperma de su pareja o de un donante en un laboratorio, fuera del cuerpo de la mujer. Una vez que el óvulo es fertilizado y se convierte en un embrión, se transfiere al útero de la mujer con la esperanza de que se implante y se desarrolle de forma natural.
Este procedimiento se utiliza en casos de infertilidad en los que otros tratamientos más convencionales, como la inseminación artificial, no han tenido éxito. La FIV también se recomienda en casos de problemas serios de fertilidad, como obstrucción de las trompas de Falopio, baja calidad del esperma, endometriosis, o cuando los intentos previos de concepción han fracasado.
El Proceso de la Fertilización In Vitro
El proceso de Fertilización In Vitro comienza con la estimulación ovárica. La mujer recibe una serie de hormonas que la ayudan a producir varios óvulos maduros, en lugar de uno solo como ocurre en el ciclo menstrual natural. Estos óvulos se extraen mediante una pequeña intervención quirúrgica bajo sedación. Posteriormente, el esperma de la pareja o un donante se recoge y se utiliza para fertilizar los óvulos en el laboratorio.
Una vez que los óvulos son fertilizados y se convierten en embriones, los especialistas monitorean su desarrollo durante unos días. Se seleccionan los embriones más sanos para ser transferidos al útero de la mujer. En algunos casos, se pueden congelar embriones adicionales para futuros intentos de embarazo.
Casos en los que se Utiliza la FIV
La Fertilización In Vitro (FIV) es una opción para parejas que han intentado concebir durante más de un año sin éxito. Los motivos para recurrir a esta técnica varían, pero entre los más comunes se encuentran:
Obstrucción de las Trompas de Falopio: Cuando las trompas de Falopio están bloqueadas, los óvulos no pueden llegar al útero para ser fecundados. La FIV ofrece una solución al fertilizar el óvulo fuera del cuerpo de la mujer y luego transferir el embrión al útero.
Endometriosis: Esta afección puede dañar los ovarios y las trompas de Falopio, afectando la calidad de los óvulos y la fertilidad. La FIV permite a las mujeres con endometriosis concebir al bypassar algunos de los problemas causados por la condición.
Problemas con el Esperma: Si la calidad del esperma es baja o hay dificultades en la motilidad del esperma, la FIV puede ser útil. En algunos casos, los médicos pueden optar por una técnica llamada ICSI (inyección intracitoplasmática de esperma), donde un solo esperma se inyecta directamente en el óvulo.
Edad Avanzada: A medida que la mujer envejece, la calidad y la cantidad de los óvulos disminuyen. La FIV es una opción viable para aquellas mujeres que desean concebir más tarde en la vida, especialmente cuando otros tratamientos no han funcionado.
Fertilidad Masculina: En casos de problemas severos de fertilidad masculina, la FIV puede permitir la fecundación de un óvulo mediante técnicas especializadas que mejoran la calidad y movilidad del esperma.
Avances en la Fertilización In Vitro
A lo largo de los años, la Fertilización In Vitro (FIV) ha avanzado significativamente. Hoy en día, los procedimientos son mucho más seguros y las tasas de éxito son más altas que nunca. La ciencia detrás de la FIV también ha mejorado, con técnicas como la criopreservación de embriones, que permite a las parejas congelar embriones para utilizarlos en intentos de embarazo futuros.
Además, el diagnóstico genético preimplantacional (DGP) ha permitido detectar posibles enfermedades genéticas en los embriones antes de la transferencia. Esto ofrece una capa adicional de seguridad para las parejas que desean evitar transmitir enfermedades hereditarias a sus hijos.
Consideraciones Emocionales y Psicológicas
Aunque la Fertilización In Vitro (FIV) ofrece esperanza a muchas parejas, es un proceso emocionalmente exigente. Las parejas que recurren a esta técnica suelen experimentar altos niveles de ansiedad y estrés debido a los procedimientos médicos, los costos involucrados y la incertidumbre del éxito.
Es fundamental que las parejas reciban apoyo emocional durante el proceso, ya sea a través de terapia psicológica o grupos de apoyo para personas que atraviesan situaciones similares. El proceso de FIV no siempre resulta exitoso en el primer intento, y esto puede ser difícil de manejar emocionalmente.
Conclusión
La Fertilización In Vitro (FIV) es una opción de tratamiento muy importante y eficaz que ha permitido a muchas parejas cumplir su sueño de tener un hijo. Gracias a sus avances en la tecnología médica, hoy en día las probabilidades de éxito son mayores, lo que proporciona a las parejas más esperanza y opciones. Aunque no está exento de desafíos emocionales y físicos, el tratamiento ha cambiado las vidas de millones de personas y continúa evolucionando para ofrecer mejores resultados.
¿Qué es el tratamiento de Fertilización In Vitro?
¿Cuáles son las indicaciones de una Fertilización In Vitro?
- Ausencia, obstrucción o lesión en las trompas.
- Disminución del número y/o movilidad de los espermatozoides o aumento de las alteraciones morfológicas de los mismos.
- Endometriosis moderada o severa.
- Alteraciones en la ovulación.
- Fracaso de otros tratamientos.
- Edad avanzada.
- Requerimiento de recepción de óvulos donados.
- Diagnóstico genético en el (los) embrión (es) antes de su implantación en el útero (PGD).
¿Cómo es el proceso antes del procedimiento?
- Evaluación del compañero o esposo que puede incluir consulta médica, examen físico y exámenes de laboratorio a criterio médico.
- Evaluación de la mujer, con su historia médica, examen físico y exámenes de laboratorio ordenados por el especialista.
¿Cuáles son las etapas de la fertilización in vitro?
¿Cuáles son los resultados de una Fertilización In Vitro?
¿Cuáles son las posibilidades de embarazo con una FIV?
¿Qué es el programa de In Vitro de cuatro ciclos?
- Medellín: Tel. +57(4) 268 80 00
- Bogotá: Tel. +57(1) 746 98 69
- Pereira: Tel. +57(6) 340 17 09
- Cartagena: Tel.+57(5) 693 0434