In Vitro Fertilization
In-Vitro fertilization is one of the world’s most widely used assisted reproduction techniques. Since 1978, when the first baby was born through this treatment, many couples have tried to achieve pregnancy through this technique that has revolutionized the world of science and human reproduction.
What is In vitro fertilization treatment?
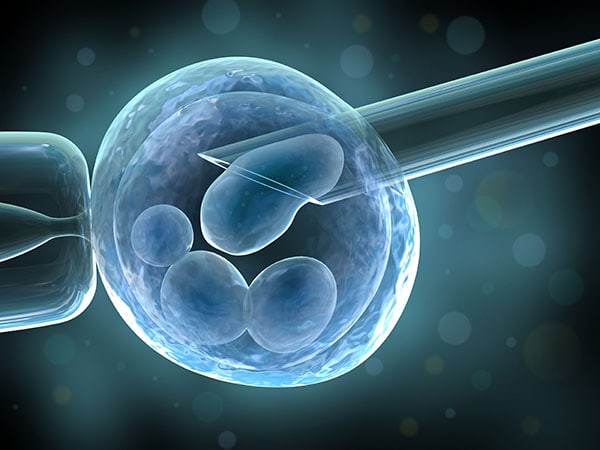
In-Vitro fertilization (IVF) is a medical treatment consisting of medical and biological procedures aimed at facilitating the union of ova (oocytes) and sperm in the laboratory to obtain embryos that will be inserted in the uterus to allow couples or women with fertility problems to conceive.
We obtain the embryos from fertilization. Embryos are the group of cells resulting from the progressive division of the ovum once it is fertilized. The goal is to generate a limited number of embryos in each treatment cycle to have reasonable chances of reproductive success.
A small number (usually 1 to 3) of the embryos obtained will be transferred to the uterus to achieve gestation. The remaining viable embryos, if any, will be stored at low temperatures (cryopreserved) for their use in the future.
What are the indications for In Vitro fertilization?
The most common indications are:
- Absence, obstruction, or injury to the Fallopian tubes.
- Decreased number or mobility of spermatozoa or increased morphological abnormalities.
- Moderate or severe endometriosis.
- Ovulation abnormalities
- Failure of other treatments.
- Advanced age.
- The requirement to receive donated eggs.
- Genetic diagnosis in the embryo(s) before implantation in utero (PGD).
What is the process before the procedure?
Before the IVF process, the doctor will perform the following evaluations:
- Evaluation of the partner or husband: may include medical consultation, physical examination, and laboratory studies at medical discretion.
- Evaluation of the woman: medical history, physical examination, and laboratory studies ordered by the specialist.
What are the stages of in vitro fertilization?
Ovulation Induction:
In-Vitro Fertilization and sperm microinjection usually begin with stimulation of the ovaries using medications, whose action is like that of certain hormones the woman produces. The purpose of this treatment is to obtain the development of several follicles, inside which the eggs are found, and to control the moment of ovulation.
Several medications stimulate the ovary, which can be administered through injections or orally.
The ovarian stimulation process is usually controlled with blood tests of ovarian hormone levels and transvaginal ultrasound that reports the number and size of developing follicles. If an adequate number of follicles reach development, other medications are administered to achieve the final maturation of the eggs.
Egg retrieval (oocyte retrieval)
The eggs are extracted by the puncture of the ovaries and aspiration of the follicles, by ultrasound guidance, and through the vaginal cavity. This is an outpatient procedure requiring sedation. The woman may go home hours after the egg retrieval with antibiotic and analgesic treatment.
The eggs retrieved are prepared and classified in the laboratory. The number of eggs extracted in the puncture and their maturity and quality varies according to the woman and cannot be accurately predicted.
Sperm Sample Collection
A sample of fresh or previously cryo-preserved and stored sperm (from the partner or donor) must be provided on the day of oocyte collection (this sample must be delivered to the laboratory within the timeframe of the oocyte uptake). The sperm sample is processed in the laboratory to separate and resuspend in the middle of the culture the best quality spermatozoa for insemination of the eggs.
Union of ova and sperm
During In-Vitro fertilization (IVF), ova and spermatozoa are placed together and incubated for fertilization to occur. It may be indicated to perform sperm microinjection (ICSI) due to significant abnormalities of the sperm analysis, previous failures of egg fertilization, or unexplained infertility with failed intrauterine inseminations. The microinjection of each ovum is performed with a sperm (IVF with ICSI), and the fertilized eggs are incubated to allow the development of embryos.
The day after IVF or ICSI, the number of fertilized eggs is determined. In the successive days of the embryo culture, the number and quality of the embryos still in development are assessed. The embryos will be kept in the laboratory for 2 to 6 days, after which the transfer will occur.
Embryo transfer
The embryo transfer involves introducing the embryos into the uterine cavity through the vaginal cavity. It is an outpatient procedure that usually does not require anesthesia. The selected embryos are then loaded into a thin probe or catheter to be introduced into the uterus through the vagina to deposit the embryo(s) inside. to make the embryonic implantation easier, hormonal treatment is prescribed after transfer.
The number of embryos transferred to the uterus is limited to one or two, and only in cases of older women or exceptional circumstances, more embryos can be transferred. Patients will receive from the biomedical team the necessary information to decide the number of embryos to transfer to optimize the possibility of pregnancy and avoid multiple pregnancies as much as possible, understanding that the ultimate and ideal goal of this process is to procure a single pregnancy that results in the birth of a child. After embryo transfer, the woman should be on embryonic rest (usually for one hour) and then can go home with hormonal treatment.
If good-quality embryos are not transferred after an In-Vitro fertilization cycle, they can be cryopreserved and stored in liquid nitrogen.
In some cases, the usual IVF and ICSI techniques may be supplemented by other procedures on gametes or embryos intended to improve embryonic implantation capacity (assisted retrieval, fragment extraction, Preimplantation Genetic Diagnosis (PGD), etc.).
The pregnancy test is done 15 days after the transfer. During this time, the woman may need to perform hormonal blood measurements to adjust the hormone replacement medication dosage.
What are the results of an In-Vitro fertilization cycle?
The factors that condition the probability of gestation in In-Vitro fertilization are:
The causes of the patient’s infertility, the woman’s age, the number of eggs obtained, and the quality of the embryos.
However, it should be considered that not all patients initiating the treatment achieve follicular development suitable for being punctured, nor do all patients with ovarian puncture have embryo transfer; this is because, in some cases, the egg collection, fertilization, or embryonic development fails. Therefore, the result of the treatment is better expressed as the percentage of gestations on the total of cycles initiated, on cycles with a follicular puncture, or cycles with transference.
80% of the gestations are obtained in the first three cycles of IVF/ICSI with successful embryo transfer; this is why discussing failed procedures with the team to discuss other treatments is necessary.
Between 40 to 60% of the patients obtain enough embryos to allow the preservation by vitrification of the unused embryos (cryopreservation), considering that the ones to be cryopreserved are those with biological viability characteristics.
When pregnancy does not occur, it is important to discuss the cycle’s outcome with the treating physician to evaluate the factors involved in the treatment process and define options for future improvement.
What are the probabilities of pregnancy with an IVF?
The probability of achieving a pregnancy with an IVF cycle is greater than 45% in women under 35. It may vary according to factors such as the woman’s age, infertility duration, and its cause. The cumulative pregnancy rate after three treatment cycles is 70 to 80%.
Age may be the most influential factor for women because the number and quality of eggs in the ovaries decrease dramatically when they are 35.
What is the four – cycle In Vitro Program?
Inser started the comprehensive program of four cycles as a very beneficial alternative on a physical and emotional level for couples since by increasing the number of attempts (4 fertilizations and embryo culture), the success rate to achieve pregnancy can grow up to 80%, something that reassures and excites the people involved in highly complex fertility treatments. One of the advantages of the comprehensive program of four In vitro cycles is that the patients, from the beginning of the program, are covered for all the possible changes that the specialist suggests to achieve pregnancy, such as embryo transfer, egg and sperm cryopreservation, fertilization through donors, etc., which means that the couple does not have to worry about extra outlays that were not established at the beginning of the treatment. In addition, InSer’s comprehensive four-cycle In-Vitro program can become a significant opportunity for emotional strengthening for the couple since proper handling of the situations inherent to the process allows the development of trust and nurtures perseverance in a common goal. In addition, it encourages personal and couple growth, improves emotional coping and effective response to unexpected results, and strengthens hope, the life project, and decision-making in common.
If you need more information about this treatment.
Contact us in our lines:
- Medellín: +57(4) 268 80 00
- Bogotá: +57(1) 746 98 69
- Cartagena: +57(5) 693 04 34
- Pereira: +57(6) 340 17 09
- Whatsapp: +57 316 3033866